Connor T. A. Brenna and Tiago C. Zortea
Is there any connection between pandemics and suicide? Unprecedented in its scale and the compensatory public health response, COVID-19 has prompted unfamiliar discussions about its likely short-term and enduring impact on physical health, mental health, and societal wellbeing.
With regard to the effect of the pandemic on suicide-related outcomes (suicide, attempted suicide, nonfatal self-harm and suicidal ideation), the academic community has advanced conflicting hypotheses. Some have suggested that suicide-related behaviours may increase, perhaps as a downstream effect of economic recession, illness anxiety, or a combination of both. Conversely, others have proposed that the extent of the threat to lives and livelihoods caused by the pandemic, and typical governmental responses to mitigate its adverse consequences for mortality and morbidity, may foster an increase in social solidarity and connectedness, either by virtue of shared hardship or by affording individuals greater time spent with family (and away from work), thereby decreasing suicide risk. These possibilities are not mutually exclusive: a short-term reduction in suicide-related outcomes might well be followed by a longer-term increase.
High-quality evidence is needed to guide both national and international responses to the pandemic, in order to understand and mitigate any potential suicide risk. To address this need, an international consortium comprising researchers from Scotland, Ireland, and Canada undertook a systematic review of the scientific literature on the effects of previous pandemics on suicide and related outcomes. The research team sought to answer the following question: What can we learn from previous “infectious disease-related public health emergencies” (pandemics) about the likely impact of the COVID-19 pandemic on the incidence of suicide and related outcomes?
Studying the Influence of Pandemics on Suicide
Collectively, our research team screened through more than 3500 article abstracts from several major scientific databases to identify 84 studies of interest. From this pool, we found only eight primary articles (i.e., presenting data) ultimately relevant to our research question. These articles, published between 1992 and 2017, examined the effects of the Great Influenza Epidemic, Russian influenza, Severe Acute Respiratory Syndrome (SARS), and Ebola Virus Disease (EVD) on suicide deaths, attempted suicide, and suicidal thoughts.
Suicide in the Context of Previous Pandemics
The eight primary studies were of mixed and relatively low methodological quality, perhaps because of challenges inherent in studying public health emergencies (for example, the absence of baseline data and lack of “experimental controls”). As a result, any conclusion drawing a causal link between pandemics and suicide-related outcomes must be heavily qualified and interpreted with caution. However, in aggregate, these studies provide evidence of a strong relationship between the SARS epidemic and increased suicide deaths among older adults studied in Hong Kong populations. Specifically, suicide rates among older adults (women, in particular) increased both during and following this 2002-2004 epidemic. A similar effect was also found among individuals with severe pre-existing illnesses, and those who were totally or partially dependent upon others for activities of daily living. Beyond SARS, we found further associations between several of the other historical pandemics and suicide deaths, attempts, and thoughts.
Drawing on the wider literature pertaining to public health emergencies and the key features of typical government responses to these (including quarantine, physical distancing, self-isolation; restrictions on movement, travel, and social interaction; and the enforced closure of non-essential workplaces, educational establishments, places of worship, and community meeting places), a more comprehensive list of likely negative psychosocial impacts in the population exposed to COVID-19 can be developed. Among these constructs are several already-established risk factors for suicide-related outcomes, including depression, anxiety, post-traumatic stress disorder (PTSD), hopelessness, fear, unresolved anger, guilt, worthlessness, sleep problems, self-stigmatisation, feelings of entrapment and burdensomeness, substance misuse, loneliness, social isolation, disconnectedness, disruption of everyday routines, unemployment, financial strain/insecurity, domestic violence, and child neglect/abuse. The potential suicidogenic impact of public health emergencies such as COVID-19 may disproportionately affect certain populations or professional groups, in particular older adults, those who are or become either unemployed or under-employed, individuals with pre-existing mental health and/or substance use disorders, and frontline health and social care staff.
Notably, the existing evidence pertaining to the timing of any increase of suicide-related outcomes in the context of a pandemic is limited. It is therefore unknown whether the impact of the COVID-19 pandemic will have an immediate or delayed effect on suicidal thoughts and behaviours, or whether the opposite effects may be seen in either time frame. Some previous research has suggested a short-term reduction in suicide rates during and immediately following natural disasters, which has been labelled as a “honeymoon period” or the “pulling together” effect, suggesting that the event may nurture or strengthen social connectedness, although the scientific findings supporting such a potential phenomenon are not consistent in the longer term. Whether or not the aftermath of COVID-19 is initially protective against suicidal thoughts and behaviours, we argue that enhanced mental health interventions will ultimately be a necessary component of the return to “normalcy”.
The articles identified by our systematic review did not examine the effectiveness of specific interventions in mitigating the impact of pandemics on the incidence of suicide, highlighting an urgent need for new avenues of research surrounding preventative measures for suicide in the context of the COVID-19 pandemic, which would inform policy-making and clinical practice. Despite this, our work constitutes the most comprehensive current knowledge on infectious disease-related public health emergencies and suicide-related outcomes, identifying gaps in the existing literature which can guide the planning and prioritisation of future research and interventions regarding suicide prevention in the context of global events.
Suicide Prevention in the Aftermath of the COVID-19 Pandemic
The emerging, preliminary evidence collected during the COVID-19 pandemic corroborates the findings of our systematic review. Preprint (shared prior to peer review) articles based on surveys of American and Japanese populations have identified a correlative relationship between suicidal ideation and COVID-19 distress (45% of study participants who endorsed suicidal ideation explicitly related it to the COVID-19 pandemic) or social distancing measures, but an overall decrease in suicidal ideation during the early stages of the global pandemic. Many researchers continue to watch with great interest, to see how these trends will evolve during a uniquely drawn-out quarantine process, and investigate how we can most effectively intervene in the lives of those who experience suicidality during and after the pandemic.
This work is driven by a recognition that suicide is not destiny. Suicide, while sometimes portrayed as inexorable, is a preventable outcome and the mental illnesses which underpin it are treatable. Although previous pandemics such as SARS left a wake of increased suicide rates, there are several suicide mitigation strategies that may result in different outcomes following COVID-19.
Mindful of the urgency in understanding and mitigating the higher suicide risk that may be expected to emerge as a function of the complex network of events triggered by the COVID-19 pandemic, a global research collaboration has been established specifically to address this issue. Supported by the International Association for Suicide Prevention, the International COVID-19 Suicide Prevention Research Collaboration aims to: share early findings and data on the impact of the pandemic and public health measures of suicide-related outcomes; facilitate research collaboration and the sharing of tools and resources; and coordinate data collection approaches. It is hoped that this collaboration will contribute to accessible and appropriately targeted research efforts, and support governments and public agencies in the global prevention of suicide-related outcomes.
The paucity of information on interventions that could mitigate the impact of infectious-related diseases on suicidal thoughts and behaviours underlines the urgent need for conducting intervention studies in the context of the COVID-19 pandemic, as such evidence would help to inform public policies of suicide prevention. Notwithstanding the dearth of such information, there are known suicide prevention strategies that could be strenghthened and amplified by governments and local authorities, which involve tackling inequalities, expanding (and creating new ways of) access to services, and both building and maintaining connectedness within communities.
Suicidal thoughts and behaviours, as well as mental health issues, are not inevitable outcomes, and there are many ways that individuals can also play an active role in the prevention process. Examples include: making regular phone calls to older adults; starting a physically-distanced exercise group; volunteering time to work with charities and those who are sick or dependent on others; checking in with loved ones and colleagues; and tending to your own mental health. The COVID-19 pandemic has undeniably represented adversity for many of us, but with strong collaborative work between individuals, communities, and governments, many lives can be saved.
Connor T. A. Brenna is a senior medical student in the Temerty Faculty of Medicine (University of Toronto, Canada). Tiago C. Zortea is a clinical psychologist and a postdoctoral researcher at the Suicidal Behaviour Research Laboratory (University of Glasgow, Scotland).
Twitter: @CTA_Brenna
Twitter: @zortea_tiago
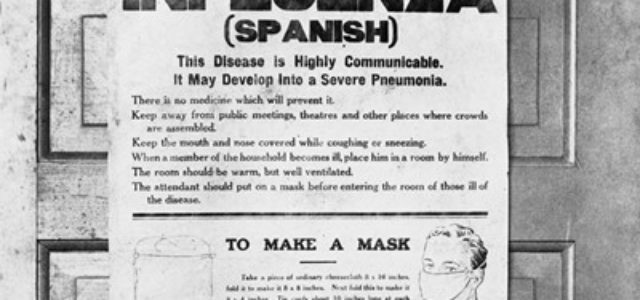
Image: 1918 influenza epidemic poster issued by the Board of Health in Alberta, Canada.