Matthew Weait (Birkbeck, University of London)
The Ebola crisis has re-ignited public debate about the way in which law should be used in the response to epidemic communicable disease. As with the relatively recent outbreaks of novel and highly infectious diseases such as SARS and zoonotic influenzas (swine and bird ‘flu), and the continuing threat posed by other viral and bacterial pathogens, the focus is – understandably – on how to strike the appropriate balance between public safety and security and individual human rights. This balance ought, where possible, to be informed solely by objective scientific evidence about risk and seriousness. It is, however, all too frequently the victim of fear, ignorance, and prejudice; of populist political posturing; and of scare-mongering reportage. The desire to assuage public anxiety through the imposition of unnecessary and ineffective coercive responses is, all too often, stoked and reinforced by a paradoxical explosion of media sensationalism – about the nature of the threat, the potential consequences, and who to blame.
All this is, of course, to be expected. In the face of danger and uncertainty, popular concerns and their expression in concrete mechanisms of control are bound to be, respectively, intense and intensified. For as long as we find ourselves confronted by a phenomenon that – for the time being at least –defeats our ability to constrain or destroy it, there will continue to be demands to “do as much as necessary” in the interests of the public and the social, whatever the cost to individual human dignity might be. The most intrusive and invasive manifestations of the precautionary principle, otherwise reserved for the exceptional case, can quickly become the norm.
More specifically, and insidiously, they will typically become the norm for some and not others. The late nineteenth and early twentieth response to gonorrhoea and syphilis – serious conditions that were impossible to treat effectively until the advent of antibiotics after the Second World War – was in many European countries to pass legislation requiring the forcible detention and testing female sex workers. Despite the fact that the circulation of these diseases was a consequence of the men who used their services, these women (and, as Elizabeth Grosz succinctly points out in her book Volatile Bodies, all women) are constructed as if they are the contaminant, “[…] regarded as a kind of sponge or conduit of other men’s ‘dirt’” (Grosz, 1994: 197).
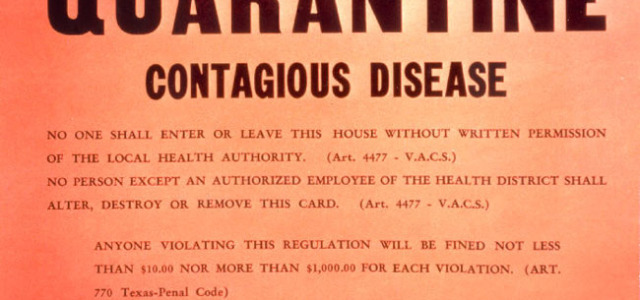
The identification of a disease with its human embodiment, and the adverse consequences of enacting and enforcing laws which reflect and reinforce this, is more than apparent in the case of HIV. Since the time the virus was identified as the causative agent of AIDS in 1983, women, Africans, and gay men have all, to varying degrees and in different ways, been identified with (and thus blamed for) a virus which, strangely enough, does not discriminate on grounds of nationality, ethnicity, gender or sexual orientation. Initially, when it was unclear what the trajectory or scale of the epidemic would be, how the virus spread and what the risk factors were, and neither vaccine, nor cure, nor treatment on the horizon, there were the inevitable, and understandable, calls for quarantine and isolation of those infected or suspected to be so (Baldwin, 2005). These calls were supplemented by demands that certain populations – those whose “lifestyle”, behaviours (such as injecting drug use or sex work), or identities rendered them morally suspect – be subject to mandatory testing. And it was only a matter of time before the criminal law was being advocated and deployed as a means of responding to those who transmitted HIV during sex, who infected doctors and dentists during surgical procedures, or mothers who passed the virus on to their infants through breastfeeding. More problematically, criminal liability was extended not only to cases where HIV was transmitted, but where there was simply exposure to the virus. The mere possibility that HIV might pass from one human to another became sufficient justification for the imposition of state punishment.
Most countries now have laws which allow for the imposition of criminal liability, under either general or HIV-specific provisions (UNAIDS, 2013). However, criminalization in practice – as evidenced by enforcement activity and convictions – has been most prevalent in the industrialised countries of Europe, North America and Australasia (Global Commission on HIV and the Law, 2012, GNP+, 2010). The justifications are both instrumental and expressive. Instrumentally, it is claimed that criminalization (especially of exposure) operates as a deterrent – both on the offender, and more generally on others, and therefore contributes to, and is beneficial for, public health; expressively, it is argued that exposure and transmission (whether intentional or unintentional) represent such serious wrongs that it is legitimate to blame and punish those who perpetrate them on retributive grounds. Both of these justifications are problematic.
As for instrumental claims there is, first, no evidence to support the contention that criminalization operates as a deterrent (Horvath et al, 2010). Second, even if it did so operate, the only people who could, logically, be deterred are those who know their HIV status. In the regions with the highest rates of criminalization, the vast majority of those who know their status are able to access, and are on, effective anti-retroviral treatment (ART); and the risk of those people transmitting HIV (because their viral load is reduced, and in most cases rendered undetectable) is significantly lower than those who are living with HIV and do not know this (Cohen et al, 2011). (In Northern Europe, it has been estimated that 90% of people on ART are undetectable, and in the United States more than three-quarters have virally suppression.) So if these people were deterred from having unprotected (i.e. condomless) sex, it would make only the most marginal difference to the spread of HIV.
Turning to expressive and retributive justifications, there is a broad international consensus that the deliberate transmission of HIV may legitimately be punished (Global Commission on HIV and the Law, 2012; UNAIDS, 2013). There is, however, a similar consensus that anything less than this should not be. For the most part it is argued that this is because the wider the ambit of criminalisation the greater the potential for adverse and unintended, disbeneficial, outcomes. Thus, if a person may be criminalised for exposure irrespective of the degree of risk which their behaviour actually involves (e.g. simply by being HIV positive and having sex which could potentially result in transmission), there is no incentive to access treatment practise safer sex (which is not, of course, to imply that there are other reasons and incentives for doing so). As regards specifically retributive justifications, these depend on being able to make a compelling case that the person has acted in a sufficiently morally irresponsible way and / or that the conduct and / or consequences of that conduct are sufficiently harmful. The problem is that in many jurisdictions, these conditions are not met. One might, for example, point to the 2008 case of Willie Campbell in Texas, who was sentenced to 35 years imprisonment after having spat at a police officer on the grounds that his spit was a “deadly weapon” (HIV cannot be transmitted through saliva). Or Nick Rhoades, who – despite having an undetectable viral load and using a condom – was originally sentenced to 25 years for exposing a man with whom he had sex to the risk of transmission. Closer to home, it currently matters not a jot that someone with HIV discloses their status to a sexual partner in Norway, and that partner consents to the risk. If unprotected sex subsequently takes place, a criminal offence is committed. (A recent Report there recommends retaining exposure liability on public health grounds – despite the absence of evidence, referred to above, that there are any public health benefits – but recommends that consent should be a defence provided that it is witnessed by a doctor …).
These examples – and there are many more – have been the impetus for a number of reform campaigns and initiatives and campaigns by activists, civil society organisations, medical professionals and scientific researchers, and international bodies, and these have begun slowly to bear fruit. The conviction against Nick Rhoades was overturned in the Iowa Supreme Court in 2014 after it heard evidence about the minimal risk his behaviour involved, and the Iowa legislature passed a Bill that, inter alia, removes criminal liability where a person “takes practical means to prevent transmission”, or discloses status to a partner and offers to take practical means but the offer is rejected. In Sweden, the country with the highest rate of conviction for HIV transmission and exposure outside North America, the Supreme Court recently upheld the acquittal of a man who had previously been convicted of reckless endangerment on the grounds that his undetectable viral load meant there was insufficient risk during unprotected sex (although, confusingly it also affirmed a previous ruling that only sex with a condom would preclude a conviction). More generally, the significance of suppressed viral load on the risk of transmission is beginning to be recognised, and publicised with the intention that this inform police, prosecutors and courts in making decisions about whether to pursue allegations (Loutfy et al, 2014; Albert et al, 2014).
HIV is, of course, a very different disease from Ebola, and global attention is, naturally, on how to respond effectively to the latter. We should not, however, be lulled into thinking that simply because it is a very different disease, the advocates of criminal liability will be disinterested in its potential application. Genital Herpes, though sharing some features with HIV (incurable, sexually transmissible), is very different in other ways (not least because it affects a significant proportion of sexually active adults). That, however, did not prevent the Court of Appeal for England and Wales upholding the conviction of David Golding for transmitting it to his partner – using the same principles that have enabled the criminalisation of HIV transmission in that jurisdiction.
And we only have to return to Texas to see that this concern is not a fanciful one. On 8th October 2014 Thomas Duncan died from Ebola in a Dallas hospital after treatment for his infection failed. Mr Duncan was making his first visit to the United States to meet his estranged partner and their son. On being informed of his death, President Obama expressed an understandable compassion for Mr Duncan’s family while also emphasising that there was very little margin for error if people and communities were not going to be put at risk. Immediately before his death, however, when there was the possibility that Mr Duncan might live, the official reaction had been somewhat less sympathetic. Commenting on the case, Craig Watkins – District Attorney for Dallas County – explained that his Office was actively considering whether criminal charges should be brought against Mr Duncan. And what precisely, as Ebola deaths reach 10,000 and the prospect appears unremittingly bleak, would have been the good of that?
References:
Albert, J. et al (2014) ‘Risk of HIV transmission from patients on antiretroviral therapy: A position statement from the Public Health Agency of Sweden and The Swedish Reference Group for Antiviral Therapy’, Scandinavian Journal of Infectious Diseases, 46: 673–677.
Baldwin, Peter (2005) Disease and Democracy: The Industrialized World Faces AIDS, University of California Press, Berkeley, and the Milbank Memorial Fund, New York.
Cohen, M et al (2011) ‘Prevention of HIV-1 Infection with Early Antiretroviral Therapy’, N Engl J Med, 365:493-505.
Global Commission on HIV and the Law (2012) Risks, Rights and Health, New York: UNDP.
GNP+ (2010) The Global Criminalisation Scan Report 2010: Documenting trends, presenting evidence, Amsterdam: Global Network of People Living with HIV (GNP+).
Grosz, Elizabeth (1994) Volatile Bodies: Toward a Corporeal Feminism, Bloomington, Indiana: Indiana University Press.
Horvath, K. et al (2010) ‘Should it be illegal for HIV-positive persons to have unprotected sex without disclosure? An examination of attitudes among US men who have sex with men and the impact of state law’, AIDS Care: Psychological and Socio-medical Aspects of AIDS/HIV, 22:10, 1221-1228.
UNAIDS (2013) Ending overly broad criminalization of HIV non-disclosure, exposure and transmission: Critical scientific, medical and legal considerations, Geneva: UNAIDS.
Matthew Weait is Professor of Law and Policy and Pro-Vice-Master (Academic and Community Partnerships) at Birkbeck, University of London. He is the author of Intimacy and Responsibility: The Criminalization of HIV Transmission (Routledge, 2007). He is currently the recipient of a Leverhulme Trust International Academic Fellowship, undertaking research into the use of expert evidence in HIV cases in the Nordic countries.